LOW BACK PAIN: SURGICAL ASPECT
by Dr AJIT N. DAMLE
The contents of this article, are related to those conditions, which often need surgical intervention, for its treatment. The other conditions are excluded, to keep the discussion related to surgery.
Most people suffer from back pain, some time or the other in life and is the second common site of pain, next to headache. Having a pain in the back is often disabling, with loss of quite a few working days and is also a financial burden on the family.
In earlier years, when the diagnostic tools were lacking ( which we realise now, having many things like ultrasonography, various types of imaging techniques like CT & MRI scan etc ) , it was more of a clinical acumen to diagnose the cause of pain in the back. Currently, imaging techniques like CT and MRI scans, Image intensifier X ray machines and Nuclear scans have made it possible to diagnose relatively early and in most of the occasions, quite accurately.
To take an overview of surgical aspects of spine surgery, it is necessary to know some basic facts of these conditions and hence are included here.
THE STRUCTURE OF SPINE:
The spine is an architectural marvel in human body. It has :
1. Multiple links, the vertebrae, which transfer the body weight and also protect the spinal cord.
2. The facets are the connecting link between the vertebrae, on the back side of a vertebra.
3. The cushions in between them, called the discs. They act as a shock absorber and dissipate the stresses well.
4. Many strong ligaments, which bind the vertebrae, yet allow good range of motion, maintaining the stability
5. The spinal cord, is continuous from lower part of the brain and is well protected in the spinal canal. In between two vertebrae, the nerve roots come on both the sides, to control various organs and the limbs.
6. The marvellous design offers stability, yet permits a good range of motion. With advancing age of a person, some age related changes do occur in the spinal column and evoke symptoms in the limbs. In the middle age, mechanical stresses may cause displacement of the contents of the disc, causing pressure on the nerves and hence pain in the limbs. The spine being a part of the body, other diseases viz. infection like tuberculosis,tumours malignancy or congenital abnormalities may also occur.
HOW DOES A CLINICIAN (medical practitioner) EVALUATE A CASE AND Some facts..
1. Spine is not that accessible from all the sides for a complete physical examination directly by vision or touch. There are a large number of possibilities of underlying conditions, which may cause given symptoms. A good and detail medical history helps to come close to a diagnosis.
2. Mechanical conditions and related diseases and fractures due to major injuries, usually occur in 30s and 40s.
3. History of vibration in work, as in a heavy vehicle driver may cause a persistent low back pain. Even those having a sedentary job, may have low back pain. What is important' is to know, if one had done any unaccustomed physical work, prior to the back pain.
4. The onset of pain may not always match with a recent physical episode of stress or unaccustomed exertion. Often a simple routinely done activity, as while sitting in a chair and forward bending to tie a shoe lace, getting in a car in awkward posture, bending over a wash basin, may trigger off low back pain.
5. Precise localisation of back pain or radiation along certain limb areas, could be difficult to localise by the patient, to convey to the clinician.
6. Pain due to infection in the spine is usually worse during the night, while that due to ankylosing spondylitis, is more in the morning hours.
Diagnostic tests:
After obtaining history, a clinical physical examination is done and usually the clinician, is able to make a provisional diagnosis, as to the cause of the pain in the back.
1. Plain x ray examination of the spine: This is a basic test, which needs to be done, prior to any other imaging tests. X ray examination with forward and backward bending helps to determine spine stability. CT scan and MRI are now available and help to detect above conditions early. ( However, one should remember false negative and false positive situations, which are known to be associated with the scans, as well.)
3. Laboratory tests are also important to confirm / exclude certain conditions. They are a great additional help in making a diagnosis.The list of various cause of pain in the low back is very long and here we would see a few common causes of low back pain, which one comes across in clinical practice and often require surgical intervention.
A. Infections: Three decades ago, infection in the spine was more common. Acute primary septic infection in spine was seen at times and had to be treated aggressively. As incidence of surgery increased, post-operative infections in the area of surgery was observed. At times, this is also observed after lumber puncture, done for administration of spinal anesthesia and is rather rare these days.
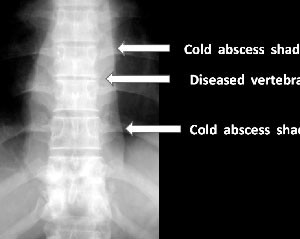
Fig.1 Spine Infection

B. Chronic infection: In developing countries, tuberculosis of lungs and intestines is observed. This may lead to secondary infection in the spine. Usual symptoms are pain more during the night. In addition, general ill health, loss of appetite and weight loss may occur. In tuberculosis of spine, observation of an abscess due to tuberculosis or loss of power in the legs could be a presenting symptom, and the patient may not complain of back pain prior to this. Hence, suspicion is very necessary for an early diagnosis. Usually, due to anatomical considerations, this disease in the lumber area (low back), is diagnosed rather late. In general, in cases who have diabetes and are HIV positive, one needs to be extra observant to come to a conclusion. When the clinician asks past history of any illness, it is prudent, not to hide history of such an infection which will help to come to a diagnosis.
Fig.2 Cold abscess around spine
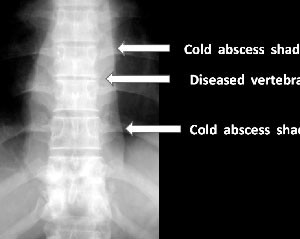
Fig.3 MRI confirms an abscess

Fig.4 Nuclear scan confirms an infection

C. Mechanical causes: Poor posture and lack of exercise, leads to altered posture. This adds to excess load on the muscles and ligaments, leading to chronic low back pain.
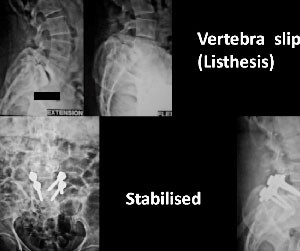
1. Congenital defect in a vertebra, may be inefficient in bearing the body load and a vertebra may slide or slowly slip, one over the other. This structural defect is between the upper and lower part of the vertebra and the spinal column above may slip forward, on the affected vertebra. The symptoms depend upon whether the spine is stable or unstable. This also leads to traction in the nerves, leading to pain along the sciatic nerve in the thighs. Such a pathological change can be associated with disc prolapse also.
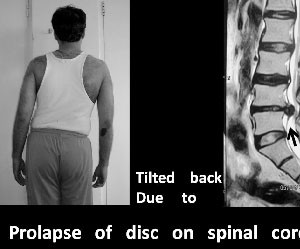
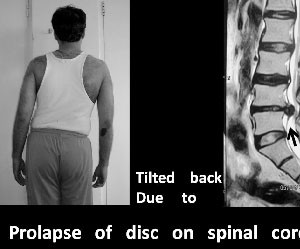
2. Prolapse of intervertebral disc: At times, due to heavy manual work, the covering ring of the disc ruptures and the contents slip out in the spinal canal, causing pressure on the nerves, leading to pain along the sciatic nerve. Initially, usually, there is bulge of the disc in the spinal canal and with continued lifting heavy weights or carrying manual work, the boundary of the disc may rupture and the contents slip out, causing pressure on the spinal cord or the nerves. Such a rupture of a disc could be seen in those leading a sedentary life also.
Fig.5 Spine tilt in disc prolapse
3. Spine canal stenosis: Stenosis means ' narrowing of a canal': In this condition, the circumference of the canal in the spinal column. The spinal cord is contained in the spinal canal. Due to changes in the structure of vertebra, ligament thickening, the circumference of the canal reduces, leading to inadequate blood supply to the spinal nerves. The usual symptoms are heaviness in the legs and progressive reduction in pain free walking distance.
4. Hyperlordosis: Such a posture with protuberant abdomen, poor posture and obesity results in narrowing of intervertebral foramina ( the side openings, through which the nerves exit the vertebral column). This pressure on the nerves, is called lateral canal stenosis. Such a situation causes pain in standing and is relieved with sitting, which involves forward bending of the spine.
5. Unstable spine: with usually forward bending of spine, increases, due to more pressure on the nerves.
6. Degeneration of the spine:
Spondylosis:
Spondylosis in true sense is a description of age related changes in the back bone. This change usually occurs after age of 45 years. The shape of upper and lower surfaces of a vertebra changes. The small joints on the back of a vertebra hypertrophy and thus the suppleness of the intervertebral joints is reduced. This leads to a relatively stiff back and some pain. The disc may extrude on a side, and compress a nerve coming out of the vertebra. It is also observed, when x ray of spine is taken, such changes are observed, but the patient have no symptoms at all and may be an incidental finding!
Fig.6 Spondylosis

7. Tumours in the spine: A tumour may occur in the spinal column or may have spread from some other site, where it started primarily.
8. Non spinal conditions: Diseases like gastro-duodenal ulcer, stone in a part of urinary system or a general illness, like a viral fever also cause low back pain.
In diagnosing a cause of such a pain, one needs to observe, if the patient is developing weakness in leg muscles, analtered or loss of sensations in some part of legs, if has some difficulty in voiding urine or motion, which is a warning sign of a serious condition.
In addition, one should also keep in mind that pain in back can be a somatic expression of an underlying tension or suppressed anxiety, which needs to be evaluated.
IN GENERAL: In general a person with disc prolapse ( sciatica) is usually a physically fit person, while that suffering from a tuberculosis of spine or tumour (either a primary or a secondary tumour) is not so. Those having degenerative disease of the spine, are also fit, but with some stiffness in the spine, with restriction of movements.
TREATMENT OF ABOVE:
In congenital defects (Spondylolisthesis means 'Slipping of a vertebra over the other') of vertebrae, usually, forward bending exercises by toning up flexors of the spine muscle and use of a corset (belt support ) helps to reduce the pain, by offering support. If such conservative method fails after adequate trial, one considers stabilisation of the spine by fusion of the affected vertebrae. About two decades ago, the vertebrae were fused by insertion of bone grafts and one had to take rest in bed for two months at least, till the vertebrae fused together, offering stability to the column. However, currently surgical technique have improved and mechanical stabilisation with metal devices called implants, permits early movements in and around the home, with an assured and good outcome.\
Fig.7 Spondylolisthesis Bone graft alone

In prolapsed intervertebral discs:
In acute herniation of the disc, initially nonoperative method is advised. It consists of:
A.Rest in bed.
B.Local warmth to the waist area.
C.Analgesics and anti-inflammatory ( pain relieving and inflammation reducing ) drugs.
D.Mild sedatives, which also relieve muscle spasm.
E.Epidural injection of steroid drug.
F.Lumber traction was commonly used, which has a good effect of offering rest in bed.
The effect: the swelling around the nerves, due to irritation by the disc is reduced, so the pain. The disc usually does not travel back to its place, but tends to shrivel. In about two to three weeks, one experiences good clinical recovery and slowly, one can return back to work.
If the symptoms do not reduce in expected duration or some weakness in muscles is noted and if this matches with the imaging modality ( M.R.I.), then one has to consider surgery of removal of the disc.
Similarly, often one gets a good relief with non-operative treatment in the first episode, but gets repeated such episodes of painful attacks. In such situations, surgical option of removal of the disc needs to be exercised.
Today, with modern imaging ( M.R.I.) technique the exact disc responsible is decided and in the operation room, the site to be operated is confirmed by use of modern 'C' arm X ray machines. These steps leads to removal the exact disc responsible for the pain. Removal of the affected disc only, is the usual procedure in the young and middle aged persons. However, in elderly, if there are symptoms of spinal canal stenosis, if confirmed by M.R.I, then a complete decompression of the spinal canal by a laminectomy ( removal of the back shield of a vertebra) and may be part of facet joints is needed. Usually, if such a procedure needs to be done in two or more vertebrae, spinal fusion ( bonding together vertebrae) is done to confer absolute stability to that segment of the spine. This is also called 'spinal instrumentation' wherein mechanical devices are used to hold the vertebrae together.
Fig.8 Listhesis stabilised by rods
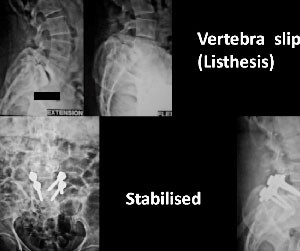
The advantages of such a procedure are:
1. Early mobilisation of the patient and prevention of muscle atrophy
2. Recurrent irritation of the exiting nerves and pain there from is forestalled.
3. Further degeneration of vertebrae and effects thereof are prevented.
4. The decision of spinal fusion is taken, taking into account, patient's age, occupation, physical requirements and few other things.
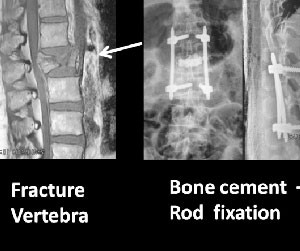
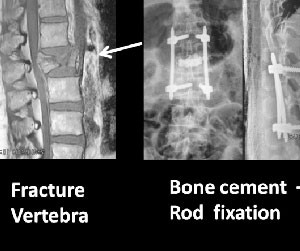
In osteoporosis of spine:
Women in general are more affected by osteoporosis, than men. This is possibly because of impact of hormonal changes in them, which affect the bone health, more than the men.
A vertebra often gets fractured, which is an insufficiency fracture. This is often, due to a trivial injury, like while travelling in a vehicle, it suddenly goes over a speed breaker, the passenger is thrown upwards and lands again on the seat. Such an impact, may cause a compression fracture in thoraco-lumber spine. Similar injury also occurs after fall in a stair or slipping on a floor and landing on buttocks.
If the bone density is somewhat good and the fracture has a sound impaction, one may be able to move about to some extent. However, if the osteoporosis is severe and the compression phenomenon is less, the fracture tends to be painful and movements also uncomfortable. In such a situation, one needs to stabilise the vertebra. This is possible by injecting bone cement in the vertebra. This is a surgical procedure, carried out in operation room.
Advantages:
1. The height of vertebra is restored and the pain reduced.
2. In some situation, in addition to this, fusion of adjacent vertebrae is also carried out.
Fig.9 Fracture spine stabilised by cement & rods
Tuberculosis of Spine:
In lumber spine, the weight bearing axis is such that, in spite of presence of infection, the person is able to move about, whereas in thoraco lumber area, the pain is quite some and the patient takes to bed early and comes early for relief of pain.
In yester years, in absence of a CT and MRI scan, the diagnosis was done on X ray film and by the time it was detected, the disease used to be quite advanced, including formation of a cold abscess. The patient would then present with a swelling of the abscess and if it has been in the spinal canal, loss of power in the legs was a presenting symptom. In such situations, evacuation of the abscesses and filling the void in vertebrae with bone grafting was a usual surgical procedure. This was followed by rest in bed for many weeks. As against this, currently the outlook has changed. Due to facilities of imaging techniques of CT, MR and nuclear scans, an early diagnosis is possible. At times a disease is detected so early that, to have a tissue diagnosis, quite often a CT guided biopsy is needed. If the diagnosis is confirmed, the current trend is that of early surgery, to remove the diseased area completely and stabilisation of the spine by metal devices. Such stabilisation permits a well aligned and stable spine. This radical approach, ( in doubtful cases) also permits having more tissue for pathological tests, to eradicate the disease completely and prevent recurrence of the disease.
Tumours and other conditions of spine are also managed in a similar way and the details are beyond the scope of the write up.