WRIST FRACTURE
by Dr Ajit N. Damle
Persons suffering from various types of arthritis do develop bone brittleness because of many reasons. This affects nearly all the bones in body and hence, it is very necessary to carry out exercises, to maintain good bone strength & joint mobility. Exercises also help to maintain balance and prevent and minimise any possibility of a fall. However, in spite of this care, still an unfortunate fall, may lead to a fracture near the wrist joint, even in a person, not suffering from any form of arthritis. This most common type of a fracture was described by Abrahm Colles in U.K. nearly two hundred years ago and is still the most common fracture, one comes across. Being a fracture in the upper limb, the person is able to move about and the hospital stay is relatively less, compared to a hip fracture.
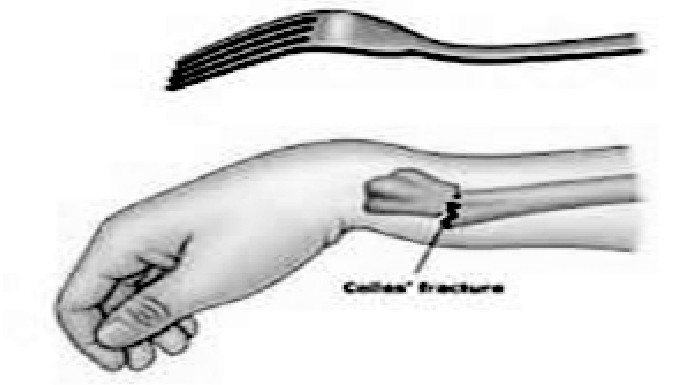
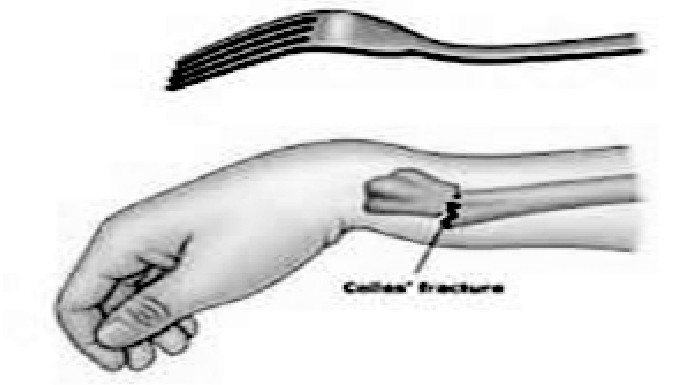
Fig 1. Deformity in wrist fracture
In a displaced fracture, the shape of the wrist resembles a dinner fork and is therefore, described very rightly, as a dinner fork deformity.The fracture may have different types injury as per fracture line geometry, seen in an X ray film and are described accordingly.
1. IMPACTED FRACTURE: In such an injury, the two fragments ( parts of the bones) are impacted in each other and hence, there is less movements in the two fragments. This confers less pain in the wrist and the shape of the wrist is not much altered. If the angulation is acceptable for a good function of the wrist and if the physical demands of the person are less, as is in an elderly person, one may accept this situation and just immobilise the wrist in a plaster cast for four to six weeks. The end result is usually gratifying.

Fig 2. Impacted fracture
1. UNDISPLACED FRACTURE:The fracture has occurred, but there is no displacement of the fragments (parts) of the bone with respect to each other. In such a case, the wrist is immobilised in a plaster cast, to maintain the bone ends in the same position. However, regular follow up and X ray examination thro' the plaster is needed every week, to confirm that the fragments continue to remain so and do not get angulated or displaced.

Fig 3. Undisplace fracture
In case one observes that they are getting displaced or angulated, then the fracture needs to be 'Set' i.e. realigned under anesthesia and small pins are inserted across the bone segments. The ends of the pins are cut off at appropriate level and the ends are buried under the skin. These pins help to maintain the fragments in place, permitting union of the bone ends. This procedure is usually carried out without taking a cut (incision) on the wrist and is called a closed procedure. Since, such a late displacement of fracture fragments is not uncommon, one may consider insertion of few pins in the bone in the beginning only and forestall the displacement of fragments, in an undisplaced fracture.

Fig 4. Fracture getting displaced

Fig 5. Fixed with pins
1. DISPLACED FRACTURE:
When the fragments are displaced at the time of injury, the wrist is obviously deformed and an x ray examination confirms the same. This demands bone setting ( reduction of the fragments and realigning them under suitable anesthesia.

Fig 6. Displaced fracture
As a standard protocol, prior to anesthesia and the surgery, certain blood tests, ECG examination and X ray chest, for safety of anesthesia are necessary. In presence of a cardiac problem, which the patient has or if it suspected by the physician, during preoperative assessment, special tests like 2 D Echo examination is advised. These steps are necessary, to prepare the patient for surgery and make the procedure safe for the patient.
At times, on arrival, the X ray examination may not define the fracture geometry and one needs to evaluate it by carrying out a CT scan examination, to plan necessary method of stabilisation of the bone fragments.
Prior treatment the patient is taking: Today, quite a few elderly persons are on drugs for diabetes or to keep the blood 'thin'. If so, one needs to consider temporary padded plaster support, till the diabetes is w ell controlled and effect of the blood thinner drug is over and the definitive procedure is safe for the patient.
The restoration of fragments is checked on the operation table and usually two pins are passed across the fracture to maintain the position achieved.
In some types of fractures, as per the fracture geometry, in addition to the pins ( wires), or instead of the pins, one may need to add a plate. This procedure of plate fixation, needs an open procedure, to realign the fragments and maintain it by fixation of a plate. Today, with advances in technology, the plates available offer more stability and help to maintain the fragments in place in a more rigid way . In a fracture, where the bone ends at the fracture area are crushed, more than expected, after realignment of fragments, a void may appear at the fracture area. In such a case, one may need to add a small portion of bone taken from the waist area bone ( Iliac crest), to fill the void in the fracture area. This is called bone grafting. This a complementary procedure, to the principle procedure and is explained to the patient and the family before hand. At times, this is not expected prior to the bone setting and the decision has to be taken during the procedure. Addition of such a bone in the fracture area, offers good contact opposition of the bone, encouraging good and assured bone union, in expected time. After the necessary type of procedure, usually one needs a plaster cast till the elbow and in certain situations, is extended above the elbow, till the mid arm.

Fig 6. Displaced fracture
POST-OPERATIVE CARE AND ADVICE:
General care and follow up:
1.The limb needs to be elevated, to keep the swelling minimum. Elevation helps to reduce the existing swelling, due to the injury and prevents further swelling coming up. A sling is used to keep the hand above the elbow.
2.Exercises for fingers, as closing and opening the grip, maintains suppleness of fingers and good grip.
3.The hand may be used for carrying out light activities, as holding a news paper, self care etc.
4.If the cast is till below the elbow, after a 2016 2016 few days, the sling should be discarded and the hand may be kept hanging down. This advice is better given by the treating surgeon, as per his protocol.
5.In any such procedure, the same side shoulder exercise is a MUST or else, one is likely to develop a stiff shoulder. As is said, prevention is better than cure, is very well applicable in such a case. This sequel is observed more commonly in a case with associated diabetes and / or arthritis.
6.Regular follow up with the surgeon is needed. As the swelling reduces, the cast may appear 'loose'. The cast does not become loose, but, it indicates that the wrist and forearm swelling is reducing well. Depending upon the individual case, the cast should be changed to a well fitting one.
Change of treatment plan:
During follow up X ray examination, a so called impacted or undisplaced fracture may be seen to get displaced and one has to reposition ( reduce) the fracture fragments, under necessary anesthesia. This is not a failure of the first method, but should be looked as a stage in total management.
Complementary drug therapy:
Presence of osteoporosis ( brittle bone) is suspected on the appearance of the wrist fracture bone structure on X ray film and by the resistance offered to the pin while being drilled in the bone. In elderly, one needs to add calcium, Vitamin D3 to the drug therapy. The blood sugar control in a diabetic patient is vital. In a case with diabetes, one may need to add insulin to be given by injection route.
Duration of plaster and long term care:
1.Fracture immobilisation is usually for a period of five to six weeks. If, due to the fracture pattern, one has offered a plaster above the elbow, after about four it may advised to reduce the plaster extent and make it till say, two inches below the elbow point. This makes the elbow free and the limb can be better used for activities of daily living.
2.After removal of the plaster cast, skin care is explained and a padded crepe bandage support is given. This helps to keep the reflex and rebound swelling coming up and offers comfort too. At this stage again, keeping the limb elevate for a couple of days is helpful. If the pins were inserted and ends buried, having a bath is permitted. Gradually, the wrist range of movement increases and wrist function improves.
3.After a few days, as the residual swelling around the wrist settles, the pin ends may become palpable and need not be source of anxiety. One continues to keep the pins as such, so the internal support is continued. One may consider removal of pins at appropriate time.
Summary:
1.Each fracture needs to be assessed on its merit and treatment planned accordingly.
2.It may be necessary to change the plan of treatment, as per follow up x ray appearance.
3.Elevation of the wrist and active exercises for fingers and the shoulder is the key to a good outcome.