Axial pain treatment

Dr.Nagnath Khadke
A quick fact to start with –
“Back pain” is the second most common medical ailment in the community after “ common cold”.
The medical management depends upon the type of back pain, whether is it – inflammatory back pain (rheumatological) or non-inflammatory (non rheumatological or mechanical).
In non rheumatological axial pain – the management varies as per the symptom duration – acute Vs chronic.
The most common rheumatological cause for axial pain is –
“ inflammatory back pain “.
Some of the other rheumatological causes of spinal pain are -
DISH (diffuse idiopathic skeletal hyperostosis)
Crystal arthropathies ( Gout / pseudogout )
Advanced Rheumatoid Arthritis / Osteoarthritis
Treatment aims of acute Non Rheumatological axial pain are –
-providing adequate information and reassurance
-providing adequate symptom control
Treatment of chronic LBP aims to:
- Minimal pharmacological intervention
- Physiotheorapy and Rehabilitation
- Improving physical abilities
- Avoiding impairment and disability
Passive treatment modalities (eg, best rest, massage, ultrasound, electrotherapy, laser and traction) should be avoided as monotherapy and should not be used routinely, because they may increase the risk of illness behaviour and chronicity.
A word of wisdom –
It is always better to not recommend “BED REST”, rather advice to stay as active as possible and to return to work early while dealing with back pain.
Pharmacological treatment of axial pain –
The treatment most commonly prescribed for back pain is medication.
-In acute LBP, drugs are prescribed, if necessary, for pain relief and to allow return to normal daily activities.
-In chronic LBP, pharmacological intervention is only for a short-term period and during pain exacerbation, to allow exercise therapy.
-Three groups of drugs are most commonly used
1) (NSAIDs),
2) Muscle relaxants
3) Analgesics
NSAIDs(Non-steroidal anti-inflammatory drugs)
- most commonly prescribed drugs worldwide
- They have anti-inflammatory action and also analgesic potential.
- Their most common side effects are Gastrointestinal complications, Cardio-vascular risk, Adverse drug reactions, potential for Renal impairment.
- Hence NSAIDs are used for short-term periods and only during pain exacerbation
A quick fact - NSAIDS relieve pain but have no effect on return to work, natural history or chronicity.
Muscle relaxants
- The term ‘muscle relaxants’ is very broad and includes a wide variety of drugs with different indications and mechanisms of action.
- Muscle relaxants can be divided into two main categories: antispasmodic and antispasticity drugs.
Antispasmodic agents - decrease muscle spasm associated with painful conditions such as iaxal pain.
- They can be subclassified into benzodiazepines and non-benzodiazepines.
- Benzodiazepines–
• are used as anxiolytic, sedatives, hypnotic agents, anticonvulsants and/or skeletal muscle relaxants.
• Their main side effects are drowsiness, dizziness and capacity to develop habituation.
• A short-acting benzodiazepine should be used as a muscle relaxant for only short periods owing to the high risk of side effects. Other pain-relieving drugs (eg paracetamol) with fewer serious side effects should be considered first.
- Non-benzodiazepines - include a variety of drugs that can act at the brain stem or spinal cord level. The mechanisms of action within the central nervous system are still not completely understood.
Antispasticity drugs - reduce spasticity that interferes with treatment or function.
Analgesics :
There are many drug groups which act as analgesics, here we are going to consider the following few.
Antidepressants
- The rationale for the use of these drugs is that they block the reuptake of neurotransmitters (eg, norepinephrine and serotonin) and so modulate pain sensations.
- They are effective in relieving pain in patients with chronic LBP, but doctors must be aware of risks.
- These drugs are not to be used in patients withrenal disease, glaucoma, pregnancy, chronic obstructive pulmonary disease and cardiac failure.
Opioids
- They can be used orally as well as can be applied through skin ( transdermal)
- Generally weak opioids (eg, tramadol, codeine, tilidin) are used to relieve pain
- Side effects are moderate (mainly constipation, dizziness or sweating, but also sexual impotence in many cases). Most side effects (except constipation) subside over time.
- Long acting weak opioids are preferred and are given regularly (around the clock) rather than as needed
Paracetamol
- Paracetamol is a preferred first choice medication for acute as well as chronic back pain, because of the effectiveness,and low risk of side effects.
- If the patient is already taking an adequate dose of paracetamol with no satisfying pain relief, then NSAIDs are considered.
quick facts
- Analgesics and NSAIDs reduce pain equally.
- Different NSAIDs or muscle relaxants are equally effective.
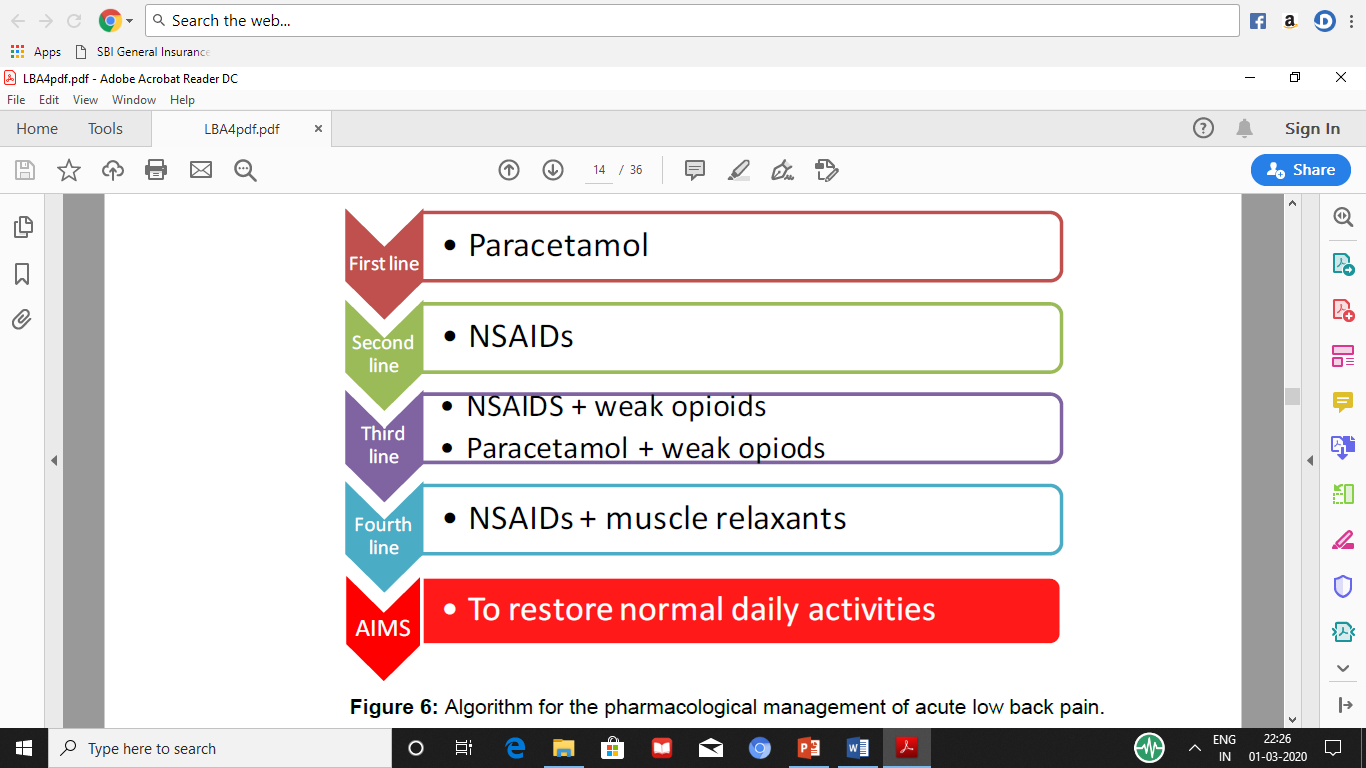
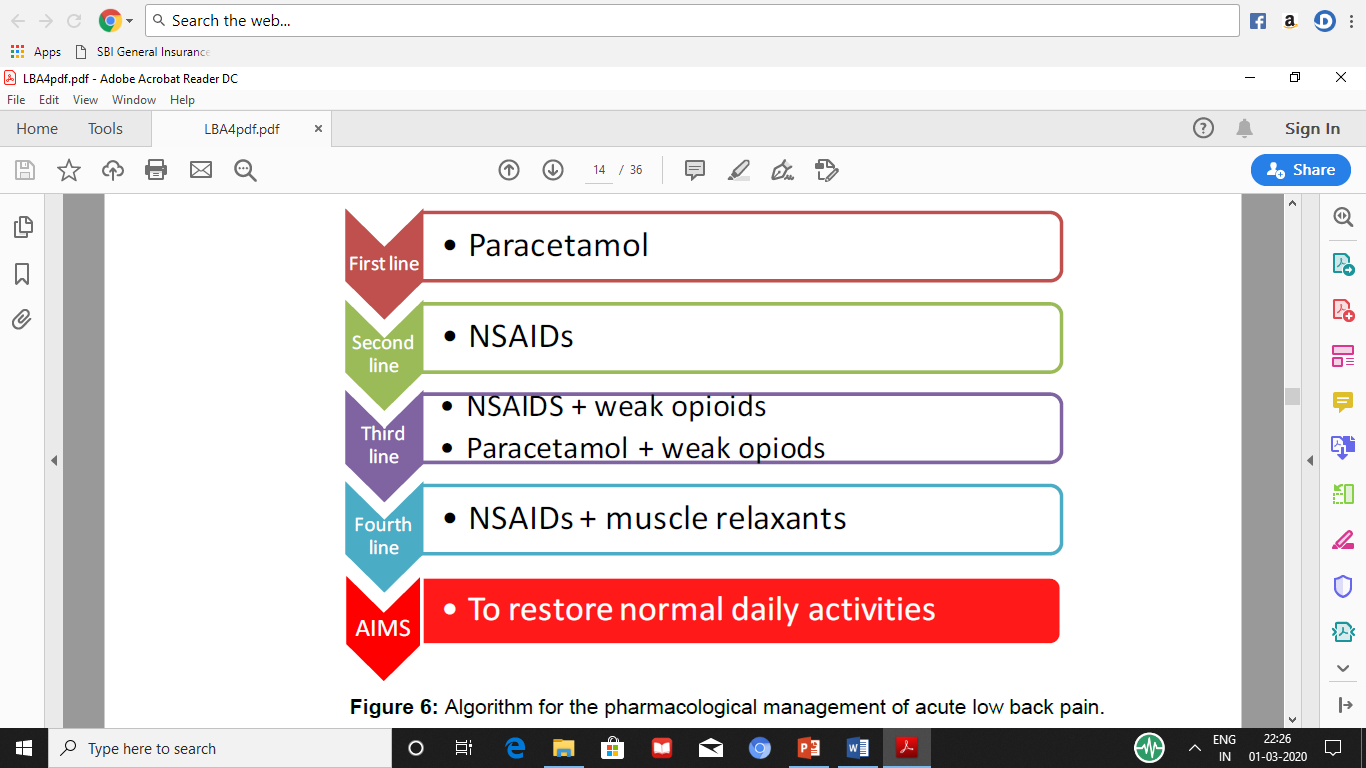
A simple algorithm for pharmacological treatment of back pain.
Rheumatological axial pain treatment
The main cause of rheumatological axial pain is, spondyloarthritis (SpA), which comprise of ankylosing spondylitis, reactive arthritis, arthritis/spondylitis associated with psoriasis and arthritis/spondylitis associated with inflammatory bowel disease (IBD).
Axial pain is common to most of them. Ankylosing spondylitis is the prototype and most common cause of axial pain.
The nature of axial pain in this diseases can be inflammatory as well as mechanical.
Inflammatory back pain is one of the most important symptom and can cause lot of impairment and disability if treated poorly. It involves both pain and stiffness.
The mechanical causes for axial pain can arise with advanced disease when the spine can get ankylosed and is at danger of spinal fractures.
Atlanto-Axial dislocation is also one of the most important cause of cervical axial pain and can be life threatening if not treated properly.
Treatment requires combination of pharmacological as well as non-pharmacological intervention.
Non pharmacological treatment mainly involves patient education / physiotherapy and regular exercise.
Pharmacological treatment of inflammatory back pain
NSAIDs are regarded as the first line drug therapy.
They decrease both pain as well as stiffness in most of the patients within 48-72 hours.
Important benefits of NSAIDs use are –
o Symptomatic control,
o facilitating regular exercise and also
o disease modifying effects.
They should be combined with gastro-protective agents to avoid GI side effects.
Furthermore, a good response to NSAID treatment is also used in a diagnostic approach to differentiate chronic back pain in patients with AS from other causes.
Normally an optimal effect of an NSAID is reached in about 2 weeks, but sometimes a longer treatment time is necessary to determine the optimal drug and dose.
They are to be used continuously rather than as and when required.
Other analgesics
These include opioids / paracetamol etc…
They are considered for paincontrol in patients with AS in whom NSAIDs are insufficient, contraindicated and/or poorly tolerated.
There efficacy in inflammatory back pain is less as compared to NSAIDs.
Corticosteroids
In contrast to the treatment of other inflammatory rheumatic diseases such as RA or systemic lupus erythematosus, systemic corticosteroids do not play a major part in the treatment of AS.
In SSA patients with dominant and severe peripheral arthritis systemic glucocorticoids can have benefit to control pain and swelling.
However axial manifestations improve only slightly, if at all, even if a relatively high dose of ≥50 mg/day of prednisolone is given.
Intravenous pulse methylprednisolone (1000 mg/day for 3 days) in patients with treatment refractory AS can have short term improvement but is not useful in long term treatment.
Conventional disease-modifying antirheumatic drugs (DMARDs)
In general, conventional DMARDs, which play such a dominant role in the treatment of rheumatoid arthritis, have no proven efficacy for the axial pain in SSA.
Sulphasalazine / Methotrexate / Leflunomide and various other DMARDs have been shown to not have any proven efficacy as far as axial symptoms are considered.
They are used many a times in cases of peripheral arthritis.
BIOLOGIC DRUGS
These are a completely new class of drugs which we have discussed till now.
These are not chemicals but protein antibodies developed with advanced techniques.
The necessity of the development of these drugs was a consequence of severely limited pharmacological treatment options for the Seronegative spondyloarthritis patients.
These drugs improve signs and symptoms rapidly and in a high percentage of patients and also reduce acute inflammation in sacroiliac joints and the spine.
They have an excellent effect on spinal pain in SSA.
Anti TNF biologic agents have been shown to be the most efficacious in the treatment of SSA.
The five Anti TNG agents approved word over are,
1) Inflixiamb
2) Etanercept
3) Certolizumab
4) Adalimuamb
5) Golimumab
There are many more agents in the pipeline as well.
These biologic agents are not without side effects though and hence the patients with best risk / benefit ratio should be considered.
There are various guidelines for recommending these drugs which need to be followed.
These guidelines also contain a strict screening for the patients desiring biologic treatment. This is necessary since Infections are one of the leading side effects of the treatment with these drugs.
Cost is another limiting factor for the use of these drugs though over the years it has reduced to a good extent.
A word of caution
Because of the complexity in the use of these drugs arising from screening, usage and possibilities of complications point of view one needs to have a complete in depth understanding of these drugs. Hence they are to be taken only with the advice and monitoring of Rheumatologists.
The mechanical causes of axial pain are many and varied.
They include causes from trauma, whiplash injury to disc herniations, myelopathy, spinal canal stenosis and spondylosis or spondylolisthesis.
The discussion of the treatment of these entities is beyond the scope of this article.