Kidneys in rheumatologic disorders
Dr.Mohini A Ganu
Though most of the rheumatologic disorders present predominantly as joint pains , connective tissue disorders like SLE, MCTD (Mixed Connective Tissue Disease), Vasculitis also involve vital organs like kidneys, brain and heart. Its important to be vigilant about internal organ involvement as the treatment plan changes according to extent of the disease.
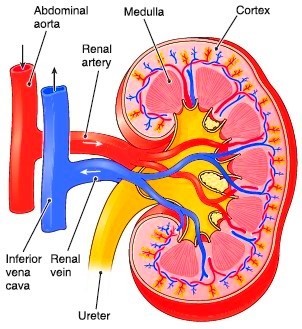
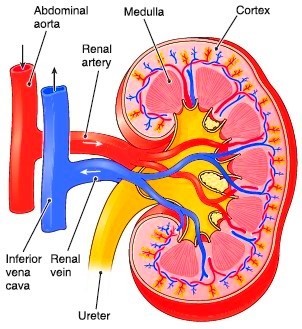
Kidneys are situated in posterior abdomen one on each side of vertebral column. Each kidney is approximately 11 to 12 cms in length, surrounded by a fibrous capsule. It is supplied by single renal artery entering through hilus which then divides into multiple branches. The renal parenchyma is broadly divided in cortex (cortex is the outside layer or covering of the kidney) and medulla. (The cortex surrounds the inside of the organ, which is called the medulla)
The functional unit of kidney is known as nephron. The number of nephrons present in the kidneys at birth is determined in foetal life. It predicts the risk of renal disease or hypertension later in life.
1.Photograph of hemisection of kidney.(Adapted from internet)
Function of kidneys- Kidneys act as garbage chutes that are essential for removal of toxic products of body metabolism. At any given time one fifth of the cardiac output perfuses the kidney. Through ultrafiltration it removes the toxic products and maintains the electrolyte and water balance.
Hypertension- Kidneys play important role in blood pressure regulation. Hypertension ( high blood pressure ) is the earliest clue to renal disease. Both renal parenchymal diseases like SLE or vasculitis with nephritsor vascular diseases affecting renal arteries eg. Vasculitis / Takayasu arteritis or polyarteritis nodosa causing narrowing of renal arteries and compromising blood supply lead to hypertension.
When do you suspect involvement of the kidneys? What are the clinical features of kidney involvement?
Main function of the kidneys is production of urine. Patients experience passing less amount of urine. Sometimes increased frequency and production of urine in excess amount is seen. Normal average urine output per day is 1 to 2 litres. If it is decreased then patients will have abnormal water retention in body leading to swelling over feet, face or whole body. Subsequently they may become breathless.
Kidneys are also required for maintaining electrolyte (sodium and potassium) balance in body. Reduced kidney function may lead to increased potassium levels in body which may in turn alter heart functioning. Reduced sodium levels either due to kidney affection or drugs used for increasing urine output cause fatiguability, reduced appetite and may affect mentation too.
Patients with kidney disease may have history of passing frank blood in urine .This may be seen in vasculitis, systemic lupus erythematosus, coagulopathies etc.Sometimes blood in urine may not be visible to naked eyes but still patient might have blood loss in urine which is visible only on microscopic examination. Hence routine urine examination is very essential for every patient of rheumatologic disorders. Patients on anticoagulants (blood thinners) have the potential danger of excess blood thinning leading to bleeding from many sites including kidneys.
In addition to blood loss patients may have protein especially albumin loss in urine. With progressive loss of albumin patients develop tendency to retain water in body leading to development of swelling all over body.
Investigations –
Urine exam is the most essential part of routine investigations of patients of rheumatologic disorders. It gives idea about infections as well as internal kidney structures that are involved. 24 hours urine collection and examination is required to assess total volume and albumin loss.
Kidney function tests i.e. Blood urea and sr. creatinine levels give idea about functional status of the kidney. Their serial estimations are sometimes required to assess progress of the disease and drug effect. These are routinely checked when patients are on DMARDs like methotrexate and immunosuppressants (eg.cyclophosphamide, azathioprine , mycophenolate mofetil).Their doses are decided accordingly.
Invasive investigation like kidney biopsy is essential to know the type and stage of kidney disease initially and sometimes for follow up subsequently.
Ultrasound examination of the kidneys reveals structural defects, fluid collection around kidneys as well as renal stones.
Complete blood counts, liver function test (LFT), Serum electrolytes and ANA pattern and profile, ANCA antibodies are few more tests required in patients suspected of kidney involvement following rheumatologic disorder.
What about treatment?
Doctors first try to confirm nature and cause of the disorder (whether it is secondary to renal stones, infections, genetic, hereditary or immunologic).
After confirming the immunologic cause doctors assess which organs in the body are involved apart from joints(lungs , heart , kidneys , brain skin etc).
After confirmation of kidney involvement drugs and doses are decided according to nature and stage of the disease.
Patients need to maintain water balance by measuring fluid intake ( water and other liquids) in 24 hours and also need to measure 24 hours urine output intermittently . This gives idea about how much water intake is to be taken. Serial body weight estimation assists in assessing fluid status and treatment effectively.
If potassium levels in blood are high then avoid green leafy vegetables, coconut water and fruits.
In order to control your blood pressure, the salt/ sodium intake should be low. It also assists in reducing the water retention in patients of chronic kidney disease. Average daily intake of sodium should be less than 2300mg/day however should be decided in consultation with treating doctor (according to stage of disease, fluid balance of body and treatment given). Canned/processed foods are to be avoided as they contain salt as preservative.
Sodium and potassium levels need to be watched meticulously in those on diuretic therapy or drugs like ACE inhibitors.
Dietary protein intake can affect renal function hence eating right amount and right type of protein is important especially in patients of advanced renal disease. Those with moderate renal function( nonnephrotic patients ) suggested protein intake is .8gms/kg/day.
Specific drugs can revert the renal disease to normal in early stages or halt the disease progression. Corticosteroids constitute essential part of treatment of nephritis (inflammation of kidneys)associated with rheumatologic diseases. To control the disease the drugs are required in higher doses. While on this drug patients may experience side effects like mooning of face, development of diabetes or hypertention and recurrent infections. However if taken under observation, side effects can be minimized while saving the kidneys from permanent damage. Never stop corticosteroids abruptly. It’s always beneficial to discuss the issue with treating doctor.
Immunosuppressants / steroid sparing drugs are also administered to control kidney disease along with corticosteroids. These drugs are needed for prolonged periods. Those with end stage kidney disease may need regular dialysis ( a process of removal of toxic products in blood through machine).
Anti hypertensive drugs are required to control raised blood pressure.
Patients have to be cautious while taking pain killers about their effects on kidneys. Unmonitored over the counter medication on your own is dangerous and should not be done.
Since treatment of kidney disease with rheumatologic cause is required on long term basis, periodic routine follow up and investigations are needed and should be done as per treating doctors advice. This will protect you from disastrous long complications of the disease and drugs.